Actinic keratosis (AK), also called solar keratosis, is considered "pre-cancerous." It has the potential to turn into a common type of skin cancer called squamous cell carcinoma. Perhaps 10% of actinic keratoses progress into squamous cell carcinoma if allowed to persist untreated over the course of several years. In transplant patients, actinic keratoses is likely to have an even higher rate of progression into a squamous cell carcinoma.
They appear as pink to red areas on the skin that often have a rough, sharp scale, similar to the feel of sand paper. They may be more easily felt than seen. Occasionally they may have a sensation of a pinprick or a burn when exposed to the sun or with any touch or pressure. They generally appear on skin that has been exposed to the sun such as the scalp, face, forearms, and back of hands.
Treatment of actinic keratoses may consist of: liquid nitrogen, 5-fluorouracil topical cream, imiquimod topical cream, photodynamic therapy, or curettage. Treatment recommendations depend on the individual patient characteristics and extent or number of actinic keratoses present.
Click here for more information.
 |
 |
 |
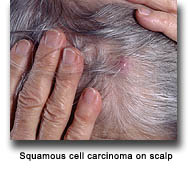
Squamous cell carcinoma (SCC) is a common form of skin cancer. It is the most common form to occur in transplant recipients. It is the second most common type of skin cancer in the non-transplant population. The risk for SCC in transplant recipients is 65 times that of the general population.
It can appear as a red, scaly bump on the skin, or an open sore that will not heal. It is often tender when gently pressed or squeezed from the side. It commonly occurs on the head, neck or back of hands, but can occur on other parts of the body. If treated early it is easily curable. If it invades deep into the skin, it can spread to the lymph nodes, requiring extensive treatment. Aggressive forms of squamous cell carcinoma that do not receive treatment in a timely manner may result in death. Squamous cell carcinoma behaves more aggressively in transplant recipients than in the general population.
Treatment can consist of electrodesiccation and curettage, surgical excision, or Mohs surgery. Very aggressive tumors may require further treatment with radiation therapy or even chemotherapy. Recommended treatment depends on the characteristics of the tumor and the patient.
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
Transplant patients are more susceptible to developing genital lesions. These lesions range from benign “age spots” to skin cancers. Viral warts due to the human papilloma virus (HPV) are common in transplant patients and HPV infection increases risk for developing SCC, particularly in the anogenital region.
Anogenital SCC most commonly appears as a slow-growing, warty lesion on the inguinal folds, genitalia, perineum, and perianal area. Organ transplant recipients of color have higher rates of HPV-induced anogenital skin cancer for reasons that are not yet understood. These skin cancers tend to have negative outcomes, primarily due to late recognition. Transplant patients should check genital skin regularly and see their doctor if new lesions arise.
Early tumors respond well to treatment with 5-fluorouracil cream. Later stage lesions may require electrodessication and curettage, surgical excision, or Mohs surgery. Similar to late stage SCC that develops on other areas of the body, aggressive tumors may require radiation or chemotherapy.
Basal cell carcinoma is the second most common form of skin cancer in immunosuppressed transplant recipients. This is different than for the general population in which basal cell carcinoma is the most common. The risk for basal cell carcinoma is 10 times that of the general population.
It appears as a small, pink, pearly bump or patch that can ulcerate, bleed, or crust repeatedly. It occurs predominately on skin surfaces that have been exposed repeatedly to the sun such as the head and neck, but it may occur on any skin surface. It is slow growing and rarely spreads to other parts of the body. If left untreated, it can lead to extensive damage and destruction of the skin and underlying structures involved.
Treatment of basal cell carcinoma may consist of electrodesiccation and curettage, surgical excision, or Mohs surgery. Radiation may also be an optional treatment. Recommended treatment depends on the characteristics of the tumor and the patient.
Note: Please click on the thumbnails below to display a larger image.
 |
 |
 |
 |
 |
 |
Melanoma is the most aggressive form of skin cancer. The risk of melanoma in transplant recipients is roughly 3-4 times that of the general population.
It usually appears as an irregular brown, black and/or red spot; or changing, unusual freckle or mole. The ABCD guidelines are promoted by the American Academy of Dermatology to assist in the evaluation of moles and the diagnosis of melanoma.




If a mole or new lesion has any of the ABCDEs, it should be evaluated by aboard-certified dermatologist. If caught in the very early stages it can be treated well with likely cure by surgical excision.
Merkel cell carcinoma is an aggressive type of skin cancer. It usually appears on the head and neck or upper extremities, as a red-purple-brown bump under the skin without an overlying open sore. It generally occurs in patients over the age of 60, however, it has been shown to occur at a younger age in transplant recipients (i.e. ~50 years of age).
Treatment of this tumor is determined on an individual basis. The tumor needs to be completely removed by excision. It is possible that your physician will sample lymph nodes in the area of the tumor to assure that the tumor has not spread to the lymph nodes. Radiation therapy may follow. Chemotherapy has been used in the past, but there is no agreement on how well it works in the treatment of this tumor. If the tumor is cut out (excised), 40% of the time it will recur in the same area that it originally appeared. Five years after a Merkel cell carcinoma is diagnosed and treated, only 30-63% of those patients are still living.
Kaposi sarcoma is a rare disorder effecting approximately 0.5% of transplanted patients in the USA. Patients of Mediterranean, Arabic, or African ancestry are especially at increased risk. Kaposi's sarcoma usually appears during the first year following transplantation and manifests as plaques or nodules on the skin and mucosae. They appear pink, red or purple in color. Skin lesions are mainly located on lower limbs, and mucosal lesions are mainly located in the mouth, but any part of the body may be involved. In some cases, it can involve lymph nodes, lungs, and gastrointestinal tract. Involvement of the gastrointestinal tract can be associated with bleeding. Kaposi's sarcoma is always associated with a specific virus (HHV8), which proliferates because of deep immunosuppression. Many cases of Kaposi's sarcoma are cured or improved by the reduction of doses in immunosuppressive treatment.
Note: Please click on the thumbnails below to display a larger image.
 |
 |
 |
|
