
Seborrheic keratosis is a noncancerous scaly growth on the skin. It is very common in those over the age of 40. Some transplant recipients appear to develop many of these growths. They can have a variety of appearances ranging in color from white to skin colored to brown to black. They all generally have a waxy scale (appearance that candle wax has been dropped on the skin.) Many appear as if they have been stuck onto the skin like a sticker or piece of bubble gum. They will occasionally peel off the skin and then re-grow. They can become irritated (itch or feel tender). They do not require treatment because they are noncancerous and noninfectious so will not spread if left untreated. If they are tender, irritated, or bothersome cosmetically, they can be removed with liquid nitrogen treatment or scraped off with a sharp instrument.
This is a type of "medical slang" used by many physicians to describe a poorly medically/scientifically characterized spot thought to be a combination of seborrheic keratosis and wart. They are scaly bumps. Often flesh colored to pink to tan in color. They tend to increase in number as the time from transplantation increases. They begin as individual spots and progress to coalesce into plaques. They commonly affect the dorsum of hands, forearms and face, but can involve the complete skin surface. Treatment is difficult, because commonly a very large surface area is involved. Moisturizers soften these scaly areas, especially a moisturizer that contains a bit of lactic acid (often 12.5%). Treatment with liquid nitrogen is effective for discrete areas of involvement. Lesions that become tender or bleed should be biopsied to rule out skin cancer.
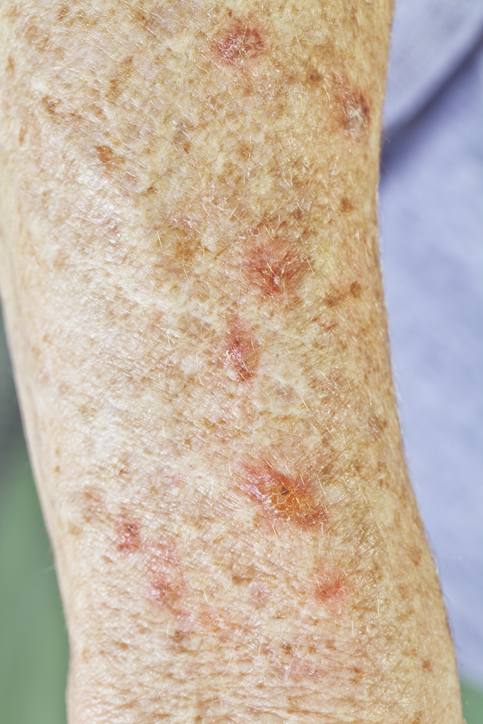
This is a spot on the skin that generally appears as an irregular plaque with central atrophy and a prominent peripheral thread-like scale. There are several different types of porokeratosis, however, in transplant recipients the most common type is disseminated superficial porokeratosis (DSP) and disseminated superficial actinic porokeratosis (DSAP). These generally occur on the extremities, especially in sun-exposed areas. They are symmetrical and can appear in crops of hundreds of lesions. Early spots may be very small scaly bumps that gradually increase in size with the peripheral thread-like scale becoming more prominent. The lesion may be flesh colored, brown or red. Many lesions may coalesce to the point that they appear just as dry skin. These can be asymptomatic or may itch and burn. They may be exacerbated by exposure to the sun. They can fluctuate in severity; spontaneously regressing or rarely progressing into a malignant variant of porokeratosis, or into a squamous cell carcinoma. Treatment options include liquid nitrogen, topical retinoid, topical immunomodulators, 5-fluorouracil, electro desiccation and curettage and rarely excision.


This is a spot that consists of prominent oil (sebaceous) glands in the skin. It appears as a yellow/orange/red bump with central indentation. Pressure to the sides of the spot may result in the expression of a yellow material. These are very common on the face. It is important to avoid application of oil containing products to the face so as to avoid exacerbation of the spots. Treatment is for cosmetic reasons and may consist of liquid nitrogen, hot cautery, curettage, excision, chemical peels and occasionally topical retinoids.
Telogen Effluvium:
This is characterized by a transient increase in the loss of normal hairs secondary to a switch in the hair growth cycles from growth phase to resting phase. It is a very common type of hair loss, especially in transplant recipients. This is caused by a major stress in one's life, such as a severe illness, high fever, major surgery (i.e. organ transplant), crash diet with significant weight loss, or childbirth. The causative event precedes the hair loss by 6 weeks to 6 months. This may continue for up to one year after the precipitating event. This is not a form of permanent hair loss. Generally full re-growth of the hair is expected and no treatment is needed.
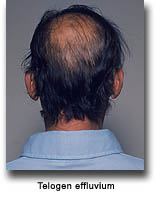

Prograf alopecia:
This is a recognized cause of hair loss in transplant recipients on Prograf (tacrolimus). It doesn't happen to every recipient taking the medication. The full nature of this type of hair loss is unknown. We do know that it is characterized by gradual hair loss resulting in thinning over the complete scalp. There is no redness or scale on the scalp. There is no breakage of the hair. It appears to not lead to complete loss of hair, but only thinning. At this time, it appears to improve only if the dose of Prograf (tacrolimus) is decreased or completely stopped. This alteration in medication for hair loss alone must be balanced with the significant benefit this medication provides the overall health of the transplant recipient and survival of the transplanted organ.
Cyclosporine is known to cause excess hair growth, and in some individuals this can be very remarkable. This hair growth can occur anywhere on the body. It is persistent while on the medication, but generally it improves when the medication is discontinued. Discontinuation of this medication is often not a good option, so other treatment for removal of the hair should be pursued. Shaving, plucking, waxing, electrolysis, and laser therapy are possible treatment options. Care should be taken with shaving, as shaving large surface areas such as the back and chest can lead to significant irritation of the skin. Electrolysis may be a concern to transplant recipients, because the procedure involves the use of small needles, and thus makes it a possible source of infection. Care should be taken to use certified electrolysis services that properly sterilize the equipment used. You may speak with your dermatologist or plastic surgeon regarding laser hair removal. You may speak with your transplant physician regarding your required medication that may be causing this. Alterations in these medications should only be taken under the direction of your transplant physician.

Acne is very common in transplant recipients. It is often caused or exacerbated by the prednisone that recipients are taking. Acne that is caused by prednisone can be difficult to treat. You should clean your face with a mild soap and water once to twice a day and use only oil-free, noncomedogenic (comedone is a type of acne lesion) moisturizers and make-ups. Treatment may consist of topical medications applied to the face daily such as topical retinoids, antibiotics, or benzoyl peroxide. Oral antibiotics may be necessary. These antibiotics must be chosen carefully so as not to interact with immunosuppressive medications that the transplant recipient is taking.

Folliculitis is inflammation of the hair follicle. It can be caused by an overgrowth of the normal bacteria or fungi living on our skin. This may occur in transplant recipients due to the immunosuppression from the medications required for the transplanted organ. Shaving can cause irritation around the hair follicles leading to inflammation. Occlusion from bandages or tight clothing may exacerbate folliculitis, as can friction. Strategies to prevent folliculitis include antibacterial soap, limit shaving or use an electric razor, shave in the direction of hair growth, and wear loose fitting clothing.
Dry skin is very common in transplant recipients, affecting as many as 75% of recipients. As you age, your skin gradually becomes drier. There are many other factors that can make dry skin worse including a dry climate, dry winter months, some illness, and various medications.

Moisturizers are key. The desired consistency of a good moisturizer is thick like that of Vaseline petroleum jelly or a traditional cold cream. A lotion that can be poured out of a bottle may contain alcohol, and have a drying effect on the skin. Choose a moisturizer that you like and use it regularly.
Dry skin can worsen and become red and itchy, despite proper moisturizing. This is often referred to as dermatitis. This should be evaluated by your physician, and corticosteroid creams may be prescribed for treatment along with moisturizers.
