Skin cancer is the most common form of all cancers. Over 1 million cases of skin cancer will be diagnosed in the U.S. this year alone. A large majority of these skin cancers are curable. Prevention and early detection of skin cancer is of the utmost importance.

Immunosuppressed patients are at a significantly increased risk of developing skin cancer. Most skin cancers are easily cured if diagnosed and treated early. However, skin cancer in immunosuppressed individuals can also be more aggressive, especially if left untreated, and has the potential to spread to other parts of the body or even cause death.
For patients with many skin cancers, the extensive and repeated treatments may result in significant scarring and disfigurement. This can affect not only the appearance of the skin but also the functional aspects of the skin and the underlying structures. Immunosuppressed patients need access to information and education related to skin cancer and its prevention. Education, prevention, and early detection of skin cancer play a key role in health and wellness.
The immunosuppressive medications that allow the transplanted organ to function and survive contribute to a patient’s risk of skin cancer. The risk of developing a skin cancer increases with increasing time from transplant. Within 10 years of organ transplant, 10-45% of transplant recipients will have a skin cancer. As many as 80% of transplant recipients will have a skin cancer after 20 years after transplant.
Some transplant recipients will have few skin cancers while others will develop hundreds of skin cancers. Skin cancer and its sequelae have been shown to have a significant negative impact on the quality of life for organ recipients. It is important for dermatologists and transplant teams to help identify an individual’s risk for skin cancer and establish surveillance by full-body skin cancer screening at appropriate intervals.
Pediatric solid organ transplant recipients also have increased risk for skin cancer, though risk is not as high as the average adult transplant recipient. Squamous cell carcinoma is most common, followed by basal cell carcinoma and melanoma. Some children develop skin cancer within a couple years of transplant, whereas for others it is delayed a couple decades. However, skin cancers in adults who had transplants as children occur at younger ages than adults who have not had transplants. Most research has focused on skin cancer risk in pediatric kidney transplant recipients. More work is needed to learn about risk for patients with other types of transplants. Overall, early and regular photoprotection are important to help decrease risk of skin cancer in children with transplants. For more detailed information, please see a 2021 review on this topic.
Published Informational Handouts
Useful Pediatric-specific Links

Patients with non-Hodgkin lymphoma and chronic lymphocytic leukemia have an increased risk of skin cancer due to impaired functioning of the immune system. Chemotherapy agents and radiation used to treat lymphoma may also increase a patient's risk for skin cancer.
In addition to a higher risk of developing skin cancer, leukemia and lymphoma patients can have a higher rate of skin cancer recurrence after surgical treatment. Patients should talk to their hematologist and dermatologist to determine how often they should have a full body skin cancer screening examination.
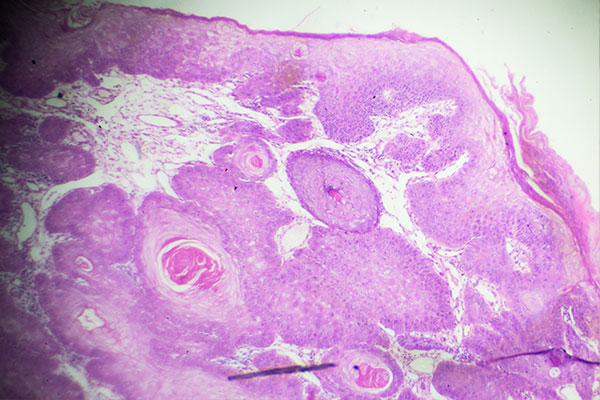 The most common type of skin cancer differs between immunosuppressed individuals and people with healthy immune systems.
The most common type of skin cancer differs between immunosuppressed individuals and people with healthy immune systems.